Undergoing knee replacement surgery can be a life-changing decision for those suffering from chronic knee pain, debilitating arthritis, or severe injury. In this guide, we delve into everything you need to know—from causes and types to the recovery process and long-term outcomes. Whether you’re a patient, caregiver, or simply researching, this article will provide an in-depth look at what to expect.
What Is Knee Replacement Surgery?
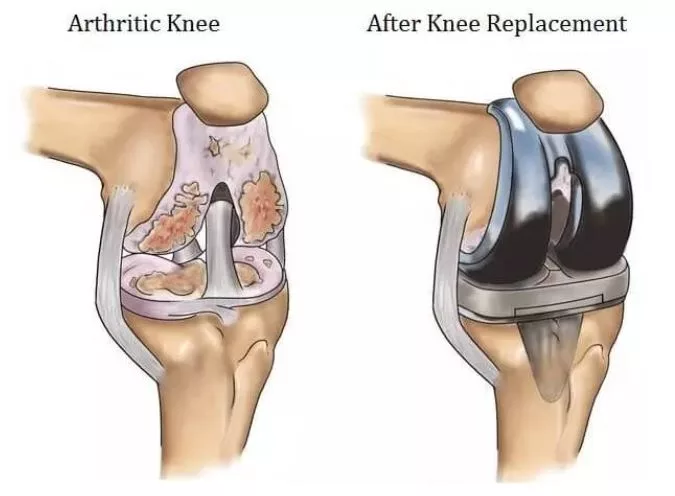
Knee replacement surgery, also known as knee arthroplasty, involves replacing a damaged or diseased knee joint with artificial components (prostheses). The primary goal is to relieve pain, restore function, and improve quality of life for individuals with severe knee conditions.
Why People Need Knee Replacement
Osteoarthritis and Rheumatoid Arthritis
Degenerative joint disease like osteoarthritis is the most common reason patients need knee replacement. Cartilage wears away over time, causing bone-on-bone friction. Rheumatoid arthritis, a chronic inflammatory condition, can also degrade joint tissue and necessitate a prosthetic solution.
Post-Traumatic Injury
Severe fractures or ligament damage that do not heal properly can lead to deformity or chronic pain, eventually requiring surgical intervention.
Other Causes
-
Avascular necrosis (loss of bone blood supply)
-
Congenital deformities
-
Failed prior knee surgeries
Types of Knee Replacement Procedures
Total Knee Replacement (TKR)
In TKR, the surgeon replaces the entire knee joint surface—typically both the femoral and tibial components, and often the patellar surface as well.
Partial (Unicompartmental) Knee Replacement
Used when only one compartment (medial, lateral, or patellofemoral) is diseased. It preserves more of the native bone and may allow faster recovery.
Revision Knee Replacement
If a prior knee replacement fails or wears out, a revision surgery is done to replace or repair the prosthetic components.
Robotic and Minimally Invasive Techniques
Advances include robotic-assisted surgical platforms and less invasive approaches that aim to improve accuracy, reduce soft-tissue damage, and accelerate recovery.
Preoperative Evaluation and Preparation
Medical Assessment
A thorough medical history, physical exam, and imaging (X-rays, MRI) help the surgeon plan the procedure. Blood tests, EKGs, and preoperative clearance from a primary care physician or cardiologist may be required.
Prehabilitation
Exercises to strengthen muscles around the knee—quadriceps, hamstrings, hip abductors—can improve postoperative outcomes.
Weight Management
Losing excess weight reduces load on the knee both before and after surgery, which may reduce complications and improve recovery.
Medication and Nutritional Optimization
Adjusting anticoagulants or anti-inflammatory medications, controlling blood sugar in diabetics, and ensuring good nutrition and hydration help minimize risks.
The Surgical Procedure: What Happens in the Operating Room
Anesthesia
Knee replacement is typically performed under general anesthesia or spinal/epidural anesthesia, often combined with a nerve block for postoperative pain control.
Incision and Exposure
A front (anterior) incision is made to access the knee joint. Soft tissues and ligaments are carefully managed to minimize trauma.
Bone Preparation
Damaged surfaces of the femur, tibia, and sometimes patella are removed. The bones are shaped to accept the prosthetic components.
Implant Positioning and Fixation
Metal and plastic components are placed. Fixation methods include bone cement (cemented), press-fit (cementless), or hybrid techniques.
Balancing the Joint
Soft-tissue releases and ligand balancing ensure the knee moves well in flexion and extension without undue tension or laxity.
Closure
After irrigation and hemostasis, the wound is closed in layers, and a sterile dressing is applied. A drain may be used initially.
Risks and Complications
While knee replacement is generally safe, risks include:
-
Infection (superficial or deep)
-
Blood clots (DVT or pulmonary embolism)
-
Prosthesis loosening or wear over time
-
Nerve or blood vessel injury
-
Stiffness or limited range of motion
-
Persistent pain or implant failure
To minimize risks, surgeons follow strict sterile protocols, use prophylactic anticoagulation, and monitor patients closely postoperatively.
Recovery and Rehabilitation
Immediate Postoperative Phase (Days 0–3)
-
Pain and swelling are managed with medications, ice, and elevation
-
Early mobilization and physical therapy begin—often walking with assistance
-
DVT prophylaxis and wound care are critical
Early Rehabilitation (Weeks 1–6)
-
Continue physical therapy: range-of-motion exercises, muscle strengthening
-
Gradually increase weight-bearing as allowed
-
Assistive devices (crutches, walker) may be used
Intermediate Phase (Months 2–6)
-
Progress to more challenging exercises, balance, and gait training
-
Return to many daily activities
-
Monitor for signs of complications such as swelling, redness, or pain
Long-Term Maintenance (6+ Months)
-
Low-impact aerobic exercise (cycling, swimming)
-
Continuing strength training and flexibility work
-
Regular check-ups with the orthopedic surgeon
Factors That Influence Outcomes
Patient Factors
Age, overall health, weight, bone quality, and muscle strength all play a role.
Implant Choice and Surgical Technique
State-of-the-art implants and accurate alignment correlate with better long-term performance.
Rehabilitation Compliance
Sticking to prescribed physical therapy and lifestyle changes is vital.
Surgeon Experience
Experienced orthopedic surgeons tend to achieve better results and fewer complications.
Expected Results: Pain Relief, Function, and Longevity
Most patients experience dramatic pain relief and improved mobility after knee replacement. Many can return to daily tasks, walking, and low-impact sports. According to long-term data, well-implanted knee prostheses can last 15 to 20 years or more when cared for properly. Some newer designs aim for even longer survivorship.
When Is Knee Replacement Not Recommended?
-
Active infection anywhere in the body
-
Severe cardiovascular or pulmonary disease posing high surgical risk
-
Poor bone stock or severe deformity unsuitable for available implants
-
Unrealistic patient expectations or inability to comply with rehab
In such cases, alternative strategies—medications, injections, braces, or osteotomy—may be attempted first.
Cost and Insurance Considerations
The cost of knee replacement surgery varies widely by country, hospital, implant type, surgeon, and postoperative care. Patients should verify insurance coverage, including hospitalization, physical therapy, and potential revision costs. Some healthcare systems and private insurers offer bundled pricing for joint replacement procedures.
Tips for Patients and Caregivers
-
Ask your surgeon about their experience and complication rates
-
Ensure clear understanding of preoperative instructions and postoperative rehab
-
Prepare your home in advance (grab bars, non-slip mats, reachable items)
-
Commit to your rehabilitation plan—progress is gradual but consistent
-
Maintain a healthy weight, diet, and lifestyle throughout recovery
Future Trends and Innovations
Emerging innovations include:
-
3D-printed patient-specific implants
-
Biologic enhancements (e.g. growth factors, stem cells) to promote integration
-
Smart implants with sensors to monitor load, alignment, and wear
-
Further development of robotic-assisted and minimally invasive techniques
These advances aim to improve accuracy, decrease complications, and extend the lifespan of prosthetic knees.
Summary
Knee replacement surgery offers a powerful solution for patients suffering from chronic joint pain and disability when conservative treatments fail. Selection of the right procedure, thorough preoperative preparation, expert surgical technique, and a well-structured rehabilitation program are all crucial to achieving a successful outcome. While risks always exist, the potential benefits—pain relief, restored mobility, improved quality of life—are substantial for many individuals.